Anesthesia: Answers to Your Questions and Fears
Hey Anesthesia, what are you doing?!
You didn’t sleep well last night because your loved one is scheduled today for a medical procedure which requires anesthesia. As the caregiver, you want to know that your loved one is safe. You offer your comforting, reassuring words, but you have fear and anxiety for your loved one’s safety.
Are your reservations about anesthesia misplaced? Are caregivers too concerned? Will my loved one sleep well while under anesthesia? The answers to these questions are simply maybe, maybe, and most likely. As someone with extensive education and experience in this space, perhaps I can allay some of your concerns. Let’s talk about anesthesia in greater detail.
What Are the Goals of Anesthesia?
When undergoing a medical procedure requiring anesthesia, there are effectively six goals for anesthesia providers to consider. All goals may not be necessary for every procedure or patient. Each anesthetic must be customized for the patient and the procedure. The listed goals are not necessarily in a methodical order.
Goal 1: Anesthesia
Anesthesia is defined as an induced state of hypnosis or unconsciousness, a sleep-like state in which temporary loss of sensation or awareness is attained. Intravenous (IV) medications or inhaled anesthetic gases are administered to achieve this state.
Goal 2: Anxiolysis/Sedation
Anxiolysis is a medical term for anxiety reduction or elimination. Certain medicines can be given to attenuate the patient’s anxiety. The most common anxiolytics are benzodiazepines, such as midazolam (Versed), lorazepam (Ativan), diazepam (Valium), alprazolam (Xanax), etc. However, medications in other classes may be used for anxiolysis.
Goal 3: Amnesia
Amnesia is a loss of recall or memory. Most patients do not want to remember their procedural experiences, so specific medications can be administered to inhibit memory formation, temporarily. You are not responsible for your words or actions while under the influence of the “good drugs.”
Goal 4: Analgesia
Analgesia is the relief of pain. Anesthesia providers can accomplish this using technical methods and numerous medications. Pain modulation is a complex topic that deserves a dedicated article. It is, unfortunately, not within the scope of this article.
Medications can be given intravenously (IV) or regionally to block pain signals to the brain. Other drugs are used to alter the brain’s perception of pain. Your anesthesia provider administers several medicines that work collectively to ease procedural pain.
The most frequently given analgesics are opioids. With the ever-concerning opioid crisis in this nation, anesthesia providers are using medications and anesthetic techniques to reduce or eliminate the need for opioids during the perioperative experience, without compromising pain control for patients. I, myself, have used such techniques with excellent results.
Goal 5: Areflexia
Areflexia is a medical term to describe a state of decreased or absent muscle reflexes or tone. Your muscles relax under particular conditions or when specific medicines are administered. That sounds scary! My heart is a muscle. Does it “relax?” No, but particular medications can depress your heart function. I am talking about the larger muscle groups in the body, i.e. skeletal muscle groups. The drugs used for the purpose of areflexia are specific to skeletal muscle fibers. Your heart is good to go! Additional agents are given to reverse areflexia.
Goal 6: Autonomic Areflexia
The implied meaning here is to control the reflexes of the Autonomic Nervous System (ANS). There are two primary branches of the ANS: the Sympathetic Nervous System (SNS) and the Parasympathetic Nervous System (PNS).
The Sympathetic Nervous System is commonly referred to as your fight-or-flight response. Your heart rate rises (tachycardia), and your blood pressure elevates (hypertension) when the bear is chasing you. A similar phenomenon occurs when you are under the knife. Go figure. If goals 1-5 did not successfully blunt your SNS reflexes, additional medicines may be provided to moderate those responses.
The Parasympathetic Nervous System is typically referred to as your rest-and-digest response. Your heart rate decreases (bradycardia), and your blood pressure declines (hypotension).
Anesthesia providers are responsible for maintaining steady vital signs during all phases of a procedure. We manipulate your ANS to keep your numbers in proper range. We don’t want numbers that are too high or too low, but just right. Arguably, the ANS is an area of the body with which anesthesia providers must be intimately familiar.
What's the Plan?
Your anesthesia provider personalizes a plan that satisfies the needs of your loved one and the medical procedure. The plan affords ideal operating conditions for the proceduralist, and the patient is optimized for the best outcome and recovery.
Keep in mind that all goals are not necessary for every patient or every procedure. For example, if a patient sustained an arm laceration requiring a repair with sutures, local or regional anesthesia may be the preferred method over general anesthesia. General anesthesia in this scenario is most likely to be excessive. It only increases the risk to the patient and adds no additional, conceivable benefit. A discussion with and an assessment by your anesthesia provider establishes the best plan for your loved one.
How Do We Reach the Goals?
There are several methods used by anesthesia providers to accomplish the set goals for the patient and procedure.
General Regional MAC Local Monitors
General Anesthesia:
General anesthesia is the most common form that patients and caregivers associate with anesthesia. It is also the most feared. General anesthesia achieves a sleep-like state in which you experience temporary loss of sensation and awareness. This is accomplished with the use of intravenous (IV) agents and/or inhaled anesthetic gases.
A breathing apparatus is frequently inserted into a portion of the patient’s airway, i.e. endotracheal tube, laryngeal mask airway, or a face mask. Patients who are under the influence of general anesthesia quite often cannot maintain their airways, so an artificial airway is established and maintained by the anesthesia provider. The anesthesia provider removes the airway device at the appropriate time.
In very rare cases, the airway must remain in place for safety reasons. Your anesthesia provider would disclose this information to you if he anticipates leaving the airway device in place. Once again, these devices are almost always removed at the conclusion of the case.
Four physiologic stages of general anesthesia exist. We refer to these stages as depths of anesthesia. They are as follows: analgesia/disorientation, excitation/delirium, surgical, and overdose.
Analgesia/disorientation:
Most patients describe sedation in this phase of the anesthetic as feeling buzzed or drunk. It is important to note that amnesia and anxiolysis are the primary goals during this stage, but they cannot be guaranteed, specifically amnesia.
Excitation/delirium:
Excitation is the next physiologic stage of general anesthesia. It is not well understood, but one theory suggests that excitatory pathways are more difficult to suppress than inhibitory neuronal pathways. At times, we see a clinical, hyperreflexic (overactive reflex) presentation of hypertension (high blood pressure), tachycardia (increased pulse rate), muscle spasticity, divergent gaze (cross-eyed), secretions, and airway spasm prior to entering a state of disinhibition (impulsivity).
Surgical:
Now, we progress to the surgical stage, which is where most patients spend the majority of time under anesthesia. It is at this depth that the patient can tolerate surgical stimulation physiologically. Stage 3 is further subdivided into 4 planes, which are not within the scope of this article.
Please note that IV inductions are used to transition the patient rapidly from stage 1 to stage 3. The excitatory stage is often encountered during inhalation induction with anesthesia gases. Excitation can also occur during emergence from general anesthesia.
Overdose:
The fourth and final stage of general anesthesia is overdose. It is possible to deepen a patient to the point of cardiopulmonary collapse, mediated by profound central nervous system depression. There are times when patients are more susceptible to overdose. Your anesthesia provider is very much aware of this possibility and titrates (adjusts) the anesthetic drugs accordingly.
Adjustments are made to the anesthetic based on the patient’s overall physical status, physiologic response, monitoring data, and a plethora of other factors. We are very careful with the medications that we use and understand that each patient requires a different dose. It is extremely rare for patients to progress to stage 4 anesthesia. Did I say, “extremely rare?”
There are also 4 described clinical phases of anesthesia care, namely, induction, maintenance, emergence, and recovery.
Induction:
Induction of anesthesia is similar to takeoff of an airplane, essentially. Induction begins after standard monitors are applied to the patient and subsequent to adequate preoxygenation with 100% oxygen. The anesthesia provider selects from a considerable number of induction agents, tailoring them to the patient.
Maintenance:
After administering these drugs and arriving in the proper plane of anesthesia, the patient then enters into the maintenance phase of anesthesia care. The proper plane of anesthesia is maintained using inhaled anesthetic gases or IV anesthetic medications.
Emergence:
Emergence is a multi-faceted endeavor to wake the patient up in a timely and elegant fashion. There is more to this exercise than simply turning the agent, gas, or IV off. Most anesthesia providers consider emergence to be more art than science. Patients expect to wake up from anesthesia and return to their normal, baseline function. That’s exactly what we do.
Recovery:
Recovery is the final phase of anesthesia. Most patients spend a designated period of time recovering from anesthesia in a Post Anesthesia Care unit (PACU). It is here where nurses continue to monitor patients for any concerns or anesthesia-related complications. If there are no concerns or complications, then the patient is discharged from anesthesia care.
Regional Anesthesia
Regional anesthesia utilizes local anesthetic drugs to block pain sensations to large, targeted areas of the body, such as arms, legs, abdomen, etc. Spinal anesthesia and epidural anesthesia are common regional, or neuraxial, techniques to numb larger portions of the body.
There are various types of regional anesthesia nerve blocks that can be performed for many surgical procedures. These blocks can be the sole anesthetic for the patient, or they can be used in concert with general anesthesia or monitored anesthesia care, i.e. moderate sedation.
Patients who receive regional anesthesia require less medications overall to keep them comfortable during the procedural experience. It is possible to eliminate the need for additional medications if a good working regional block is in play, thereby mitigating the associated risks of those medications.
It is important to note that regional anesthesia carries risks as well, some of which can be substantially serious if they occur. Most anesthesia providers agree that regional anesthesia carries less overall risk as compared to general anesthesia.
Monitored Anesthesia Care (MAC)
Monitored Anesthesia Care is a service provided to patients who do not require complete unconsciousness for a given procedure. Often times, medications are used to sedate the patient to varying levels of consciousness, without progressing to general anesthesia. There is a well-described continuum of depth of sedation, ranging from minimal to deep.
The term “conscious sedation” is what most people understand as MAC. Amnesia cannot be guaranteed with this particular method. Moderate sedation combined with a strategic regional anesthetic can make for a pleasant patient experience.
Local, Local, Local
Local anesthesia uses medicines to numb smaller areas of the body. Typically, the local medication is given as a one-time injection into a small area, such as a finger, skin, or laceration. Patients undergoing a procedure with local anesthesia should not feel pain, but they still may feel pressure. Often times, sedation is given in addition to the local injection. Local is regarded as the safest type of anesthesia.
Monitors
Standard monitors are applied to patients receiving any type of anesthesia. You can expect blood pressure, pulse oximetry, and EKG monitoring. End tidal carbon dioxide (ETCO2) and temperature are also routinely monitored. The procedure or patient’s health may dictate utilization of more invasive monitors.
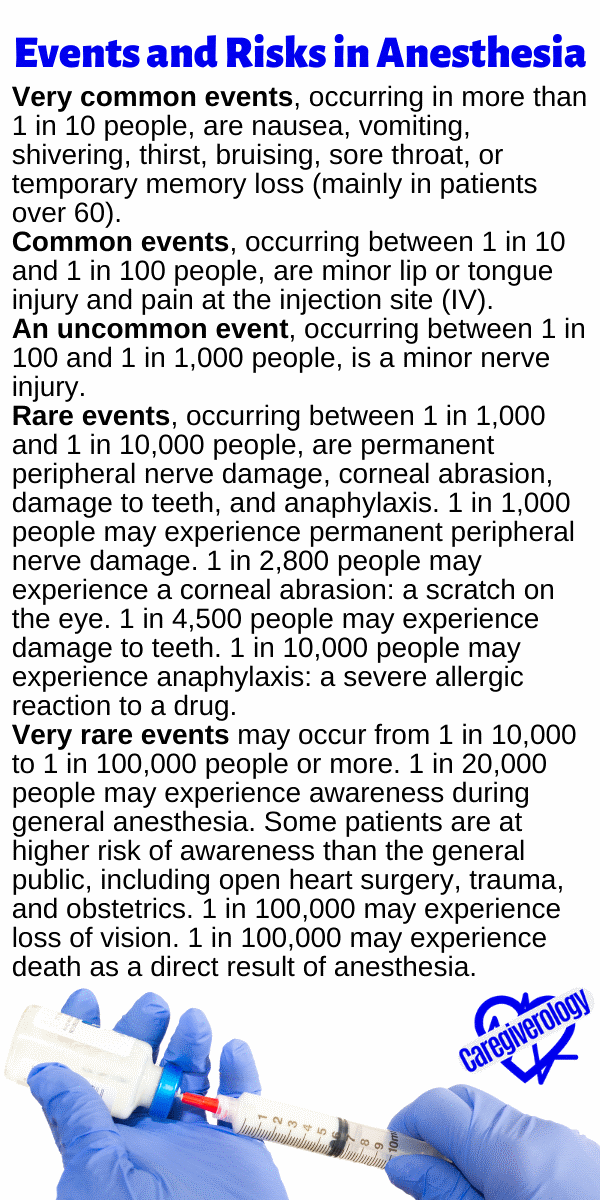
Events and Risks in Anesthesia
Very common events, occurring in more than 1 in 10 people, are nausea, vomiting, shivering, thirst, bruising, sore throat, or temporary memory loss (mainly in patients over 60).
Common events, occurring between 1 in 10 and 1 in 100 people, are minor lip or tongue injury and pain at the injection site (IV).
An uncommon event, occurring between 1 in 100 and 1 in 1,000 people, is a minor nerve injury.
Rare events, occurring between 1 in 1,000 and 1 in 10,000 people, are permanent peripheral nerve damage, corneal abrasion, damage to teeth, and anaphylaxis. 1 in 1,000 people may experience permanent peripheral nerve damage. 1 in 2,800 people may experience a corneal abrasion: a scratch on the eye. 1 in 4,500 people may experience damage to teeth. 1 in 10,000 people may experience anaphylaxis: a severe allergic reaction to a drug.
Very rare events may occur from 1 in 10,000 to 1 in 100,000 people or more. 1 in 20,000 people may experience awareness during general anesthesia. Some patients are at higher risk of awareness than the general public, including open heart surgery, trauma, and obstetrics. 1 in 100,000 may experience loss of vision. 1 in 100,000 may experience death as a direct result of anesthesia.
Please keep in mind that normal life tasks, like driving a car, are statistically riskier than the very rare events listed above. Modern anesthesia is overall very safe. Anesthesia providers take great care to minimize complications. The above listed events and risks are not exhaustive; other complications exist with specialized anesthesia techniques that are not discussed in this article.
Your loved one can sleep well knowing that he or she is receiving the best anesthesia care, practiced with the utmost discipline and vigilance. We are there every breath, every beat, and every second. Rest easy. Sleep well.
Bryan Tanner, MSN, APN, CRNA
Guest Articles Written for Caregiverology
Medical References and Resources for Caregivers
From Anesthesia: Answers to Your Questions and Fears to Home
Recent Articles
-
Lifestyle Medicine Explained: Guiding You Back to Better Health
Apr 20, 25 09:51 AM
Did you know that 80% of chronic diseases—like heart disease, diabetes, and obesity—are preventable through lifestyle changes? Yet, many people rely solely on medication rather than addressing the roo… -
What to Expect During Post-Operative Recovery at Home - Caregiverology
Apr 08, 25 08:21 PM
Surgery may be over, but the journey to full recovery is just beginning, and for many people, the hardest part happens after they leave the hospital. -
How to Plan for Aging: Financial, Health, and Lifestyle Considerations
Mar 29, 25 12:40 PM
Did you know that 70% of people over 65 will need some form of long-term care? Yet, many delay planning until it’s too late. Aging is inevitable, but how we experience it depends on preparation.




New! Comments
Have something to say about what you just read? Leave a comment in the box below.