Changing the ER / Hospital to Better Assist Dementia
What protocols do hospitals have in place when a person comes into the emergency room (ER) who has severe dementia? This article is an attempt to raise more awareness to ER and hospital settings, some that often have NO clue what is coming! As a caregiver of someone with dementia, there are many suggestions I'd like these facilities to think about.
What's coming Arrival Deescalate Family Time Experience Questionnaire Form
So What IS Coming?
The scenario may be of a patient being out of touch, highly agitated, or experiencing hallucinations of being hurt by someone. What would be their approach to this scenario? Does their staff have adequate training on how to deal with these types of patients? I realize they have training but the question is that is it enough training?
Many people do not realize that there are over 50 million people with dementia worldwide and that nearly 10 million more new cases show up each and every year! The aging baby boomer generation will continue to increase this statistic over the next few decades. How prepared are most hospitals? Are they ready for the influx in care when they arrive in their setting?
I believe extensive geriatrics education, including Alzheimer's and dementia care, should be mandatory for all health care staff. Staff needs to know what to say and how to understand them. What is the dementia individuals reality at the moment? It's usually not in the present day. Adapt their care approach with calm voices, slower speaking skills, reassurance, maybe calm music on a headset. It is often simple things that make a big difference.
Arrival to the Emergency Room
When a person enters the emergency room doors in a disoriented and often combative state, it could be due to the stage and type of dementia they are dealing with. It could be due to a side effect of the medications they are taking. It could also be due to an infection such as a urinary tract infection (UTI).
Most aren't able to communicate exactly what they are feeling. Many of them are either in pain, scared, or both. In one sense, it's almost like having a person with a mental condition similar to schizophrenia or bipolar disorder come in, except the focus is primarily about behavioral issues.
They may get more agitated and scared when they have a load of people piling into their room, asking all these questions, hooking up blood pressure cuffs, etc. Bright colors, bright lights and a lot of hoopla going on bothers them and escalates their condition, especially upon first arrival.
How to Deescalate the Situation
Most of the time when they are brought in it's because they need help deescalating. How to do this is often unclear. Every patient is unique and what works for one may not work for the other. Unfortunately, a clear path is not always immediately attainable.
The solution may be to put them on a medication to help them calm down or they may just need a medication adjustment. Oftentimes they could be having a negative side effect to a new medication they have been put on. So many antipsychotic medications alter their brain function in a negative way.
Another possible solution is to have a quite room in the ER that has less lighting and softer colors on the walls, as well as the sheets being more neutral in color. A room that is more like a home bedroom similar to what the maternity wards have. A warm and inviting setting can often calm their nerves.
Family Can Often Help
If there is a family member with them that can articulate that their loved one has dementia, they need to be the ones that speak with the staff. The patient can not always give truthful answers, as they often do not understand the questions asked. I'm not saying to simply ignore the patient as they still need to be treated humanely and with "kid" gloves. They are still human and not be seen as just another person with dementia.
Something else to consider, if they are admitted into the hospital, is to ask a family member to stay overnight with them. If the disease hasn't progressed to the point of them not recognizing their family members, keeping them around and hearing their voices can cause them to be calmer.
Time is of the Essence
Another huge issue at many ERs is the time it takes for them to be seen. Time is of the essence as the longer they are out of their normal setting, the worse the confusion gets. As the time passes, they often get even more out of hand. Because they aren't considered to be in a level that is a true emergency, they are often made to wait in the waiting room for a longer period of time compared to many other patients coming in.
I realize health care oftentimes has a lack of staff, but there has to be a solution to be able to move dementia patients quicker through the ER process. Possibly just a quite room to begin with, maybe a camera to observe the demented individual. This could help them to be less anxious when they are observed by nurses and doctors.
In a perfect world, it would be great if doctors made house calls or did video visits, so that we as family and caregivers didn't have to subject the demented individual to the ER unless the situation is a true emergency! Although there have been some advances towards this, it isn't very widespread as of yet.
A Heartbreaking Experience
I witnessed a situation where a gentleman was admitted to a hospital and felt abandoned when the nurses left him alone. He would get really frightened. He honestly had no idea where he was. He kept trying to get out of his bed and would have fallen if he succeeded because he was so unsteady. I told him to stay in his bed but he was determined and just became more frustrated.
Then his meal came and they set his tray near him and left the room. He wasn't able to communicate well, but I could see he couldn't move his utensils to his face. I called a nurse and no one had time to feed him right then. She said he would have to wait awhile. After 10 minutes, I thought oh heck I'll go help him. About that time, an aide came in. I told her he needs assistance to eat. She made a note in his chart.
At this point, he was no longer interested in his meal as it was cold and gummy. Shortly after the kitchen staff came and took his tray away stating that he didn't eat much. This made me a lot more aware of how lacking the training is for dementia patients. I also observed no staff checking on him in over two hours.
I am not sure what the answer is, but this gentleman didn't have family that wanted to stay with him. They just dumped him, figuring he'd be getting the best of care. He didn't know how to push the call button either, even though the aide said here's your call button, with no explanation of how to use it properly. Such a sad memory!
I am aware that this was just one scenario but I'm sure there have been many others that were very similar. I realize that no facility is perfect and I know that most of the staff are doing their very best. But at the same time, I see a window of opportunity to make these patient's experience better. All facilities should be constantly striving to improve regardless of how positive the experience is already.
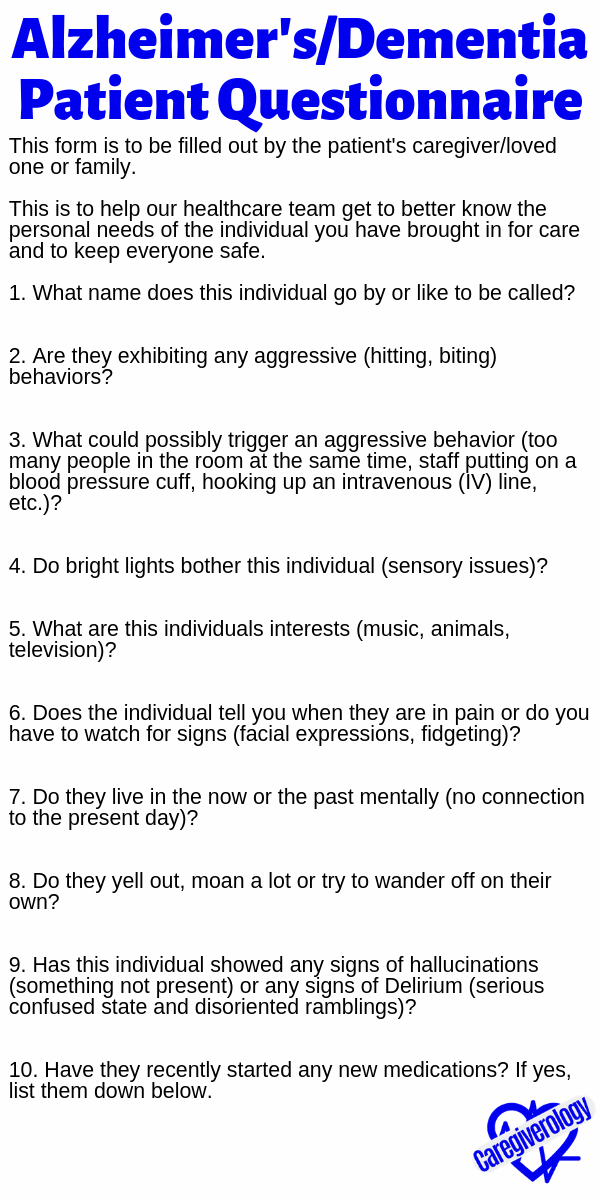
A Standardized Questionnaire?
When an individual with dementia enters a hospital setting, I believe a standardized form should be made available to the family or caregiver to fill out regarding the patient. Questions such as:
- Does the person go by a nickname?
- Are they living in the moment right now? A lot are not in the present day.
- What causes triggers that lead to more agitation or aggressiveness? Noises, lights or someone coming at them to fast.
- What are some dislikes and likes this individual may have?
- Do they have signs they show of being in pain or discomfort, especially if they aren't very verbal?
- Do they like to wander?
- Do they yell out at night?
The form down below can be printed or mailed out to local hospitals. It lists these questions and more. I believe it will help the staff better understand the incoming dementia patient more thoroughly. If the medical professionals, especially in hospital/ER settings, are not fully equipped for the influx of individuals diagnosed with Alzheimer's disease and dementia, what will this say about out healthcare system? These patients need to be understood to the best of our ability. Let's help be the change!
Dementia/Alzheimer's Disease Patient Questionnaire
This form is to be filled out by the patient's caregiver/loved one or family.
This is to help our healthcare team get to better know the personal needs of the individual you have brought in for care and to keep everyone safe.
- What name does this individual go by or like to be called?
- Are they exhibiting any aggressive (hitting, biting) behaviors?
- What could possibly trigger an aggressive behavior (too many people in the room at the same time, staff putting on a blood pressure cuff, hooking up an intravenous (IV) line, etc.)?
- Do bright lights bother this individual (sensory issues)?
- What are this individuals interests (music, animals, television)?
- Does the individual tell you when they are in pain or do you have to watch for signs (facial expressions, fidgeting)?
- Do they live in the now or the past mentally (no connection to the present day)?
- Do they yell out, moan a lot or try to wander off on their own?
- Has this individual showed any signs of hallucinations (something not present) or any signs of Delirium (serious confused state and disoriented ramblings)?
- Have they recently started any new medications? If yes, list them down below.
Download and print this form here (pdf)
Pin this form!
Thank you Gayle Yarbrough for contributing this article.
Stages and Types of Dementia: In Depth Overview
Late Stage Alzheimer's Disease Care Tips
Guest Articles Written for Caregiverology
From Changing the ER / Hospital to Better Assist Dementia to Home
Recent Articles
-
Common Truck Crash Injuries and Legal Remedies - Caregiverology
Jul 19, 25 10:49 AM
Known for its sun-drenched beaches, vibrant arts scene, and bustling maritime industry, Fort Lauderdale is a city that sees heavy traffic both on its roads and at its busy port. Unfortunately, with th… -
Why Expert Legal Help Matters After Serious Injury - Caregiverology
Jul 19, 25 10:35 AM
In Houston, over 67,600 car crashes occurred in 2023, resulting in 290 fatalities and 1,612 serious injuries. That’s roughly 185 accidents every day. -
How Life Care Planners Support Injury Recovery - Caregiverology
Jul 19, 25 10:18 AM
In Los Angeles, life care planners play a vital role in supporting injury recovery, especially for individuals facing catastrophic injuries such as traumatic brain injuries or spinal cord damage.




New! Comments
Have something to say about what you just read? Leave a comment in the box below.