What Does Fall Risk Mean?
Patients who are considered a fall risk have a higher risk of falling than others and should have extra precautions taken to make sure they are safe. The older a patient gets, the more likely they are to fall and injure themselves. If they must ambulate, they may require a cane, walker, or sara stedy. They may not be allowed to get up at all if they are on bedrest.
Yellow Elderly patients Young patients Nighttime Morse Tips Pin

The Color Yellow
In the hospital where I am employed, the color yellow represents patients who are considered to have a high risk of falling. Many are considered a risk as soon as they are admitted. If they get this diagnosis, they are assigned to have a yellow sign in front of their door, a yellow arm band that has "fall risk" on it, and yellow double-sided slip-resistant socks.
This is a very useful way to identify people who you need to be extra cautious with. If you work in a facility that doesn't use this or a similar method for high risk patients, it may be a good idea to mention that they should start. It will more than likely prevent many falls from happening in the future.
 Double-sided slip-resistant socks
Double-sided slip-resistant socksElderly Patients Have The Highest Risk
Elderly people fall a lot more often than younger ones. This may not seem like a big deal at first but it certainly is. A younger person can fall and get right back up. An elderly person almost always needs help in order to get back up. Sometimes, help isn't always there right away.
The person may be on the ground for hours, or if they live by themselves, even days. When this happens, they may not be able to reach a phone to call for help or may even become unconscious. Either way, this is not a situation anyone should be in.
This scenario is so common that there are many different medical alert devices available. The device is a simple button worn around a person's wrist or neck. That way they always have it with them in case of an emergency. When the button is pressed, it immediately alerts emergency services. This has literally been a life saver for so many people.
I have taken care of many patients who have broken their hip or knee because of a fall. I've even taken care of a few who had a concussion. These things not only have to be repaired, often with surgery, but they also take a long time to heal.
Research has shown that once a patient falls once, there is a much higher probability that they will again in the near future. And of course, the older they are, the more this statistic applies to them. The longer a patient goes without falling, the less falls they will likely have altogether.
Be Mindful Of Younger Patients Too
To a certain extent, you should consider all of your patients to be a fall risk. This may sound silly but it's better to be safe than sorry. Even if a patient is completely alert and mobile, when they receive various medications such as pain medicine, they often become disoriented and unstable.
On top of being drowsy from pain medicine, they may also have an iv line or port connected to them along with a heart monitor, oxygen tubing, pulse oximeter, a foley catheter, and a sequential compression device. All of these things have to be taken off a certain way. If the patient jumps out of bed without thinking, these things can easily cause them to trip and fall.
Be Extra Aware At Night
Patients are at an even higher fall risk at nighttime. Patients with dementia often wake up and immediately try to get up. Luckily, if they have a bed alarm or chair alarm on, you will be able to rush into the room and prevent them from falling. These alarms have prevented countless falls for me.
Even patients without dementia have told me that they forgot they were in the hospital after waking up from a deep sleep. This goes to show that you can never be too careful. If a patient needs assistance to get up, it is best to turn their bed alarm on at night regardless of their mental status.
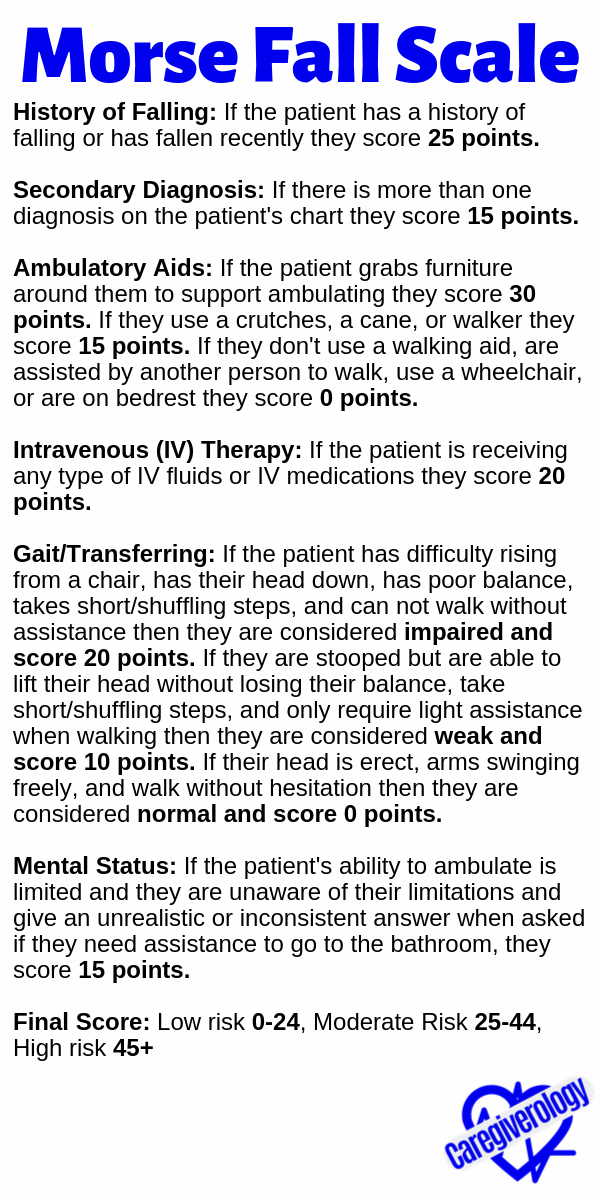
Morse Fall Scale (MFS)
History of Falling: If the patient has a history of falling or has fallen recently they score 25 points.
Secondary Diagnosis: If there is more than one diagnosis on the patient's chart they score 15 points.
Ambulatory Aids: If the patient grabs furniture around them to support ambulating they score 30 points. If they use a crutches, a cane, or walker they score 15 points. If they don't use a walking aid, are assisted by another person to walk, use a wheelchair, or are on bedrest they score 0 points.
Intravenous (IV) Therapy: If the patient is receiving any type of IV fluids or IV medications they score 20 points.
Gait/Transferring: If the patient has difficulty rising from a chair, has their head down, has poor balance, takes short/shuffling steps, and can not walk without assistance then they are considered impaired and score 20 points. If they are stooped but are able to lift their head without losing their balance, take short/shuffling steps, and only require light assistance when walking then they are considered weak and score 10 points. If their head is erect, arms swinging freely, and walk without hesitation then they are considered normal and score 0 points.
Mental Status: If the patient's ability to ambulate is limited and they are unaware of their limitations and give an unrealistic or inconsistent answer when asked if they need assistance to go to the bathroom, they score 15 points.
Final Score: Low risk 0-24, Moderate Risk 25-44, High risk 45+
0 789+MS 456–M+ 123×M- 0.EXP÷MR ±√xC=MC |
| powered by calculator.net |
Some Final Tips
If the patient has poor vision:
- Make sure they are wearing their glasses before they get up
- Have adequate lighting while ambulating
- Keep a night light on at night including one near the bathroom
- Keep everything needed within reach of the bed such as glasses, phone, call light, dentures, etc.
If they have poor balance or generalized weakness:
- Discourage them from stretching or bending down to reach things
- Wear skid resistant socks or shoes, especially if they are wearing ted hose stockings
- Use walking aids such as canes and walkers
- Lock wheelchair wheels before getting in or out of them
- Avoid wearing clothing that is too loose that may result in a tripping hazard
- Avoid wearing clothing that is too tight that may reduce movement of the extremities
Be aware if they are taking medication, especially newly prescribed ones such as:
- Pain killers
- Tranquilizers
- Antidepressants
- Sleep aids
- Heart and blood pressure pills
Be mindful of and possibly eliminate:
- Liquid on the floor from leaks or spills
- Tubes, wires, and cables that are in walking areas
- Loose or wrinkled floor mats, none at all is best
- Other obstacles around areas frequently walked on such as around the bed and bathroom
Pin this article!
From What Does Fall Risk Mean to Home
Reference:
http://www.networkofcare.org/library/Morse%20Fall%20Scale.pdf
Recent Articles
-
Common Truck Crash Injuries and Legal Remedies - Caregiverology
Jul 19, 25 10:49 AM
Known for its sun-drenched beaches, vibrant arts scene, and bustling maritime industry, Fort Lauderdale is a city that sees heavy traffic both on its roads and at its busy port. Unfortunately, with th… -
Why Expert Legal Help Matters After Serious Injury - Caregiverology
Jul 19, 25 10:35 AM
In Houston, over 67,600 car crashes occurred in 2023, resulting in 290 fatalities and 1,612 serious injuries. That’s roughly 185 accidents every day. -
How Life Care Planners Support Injury Recovery - Caregiverology
Jul 19, 25 10:18 AM
In Los Angeles, life care planners play a vital role in supporting injury recovery, especially for individuals facing catastrophic injuries such as traumatic brain injuries or spinal cord damage.




New! Comments
Have something to say about what you just read? Leave a comment in the box below.