Pain Management Basics for Your Patient
Pain management for your patient can be a very touchy and controversial topic. It is difficult to diagnose and sometimes impossible to manage completely. It is experienced and often managed differently from person to person.
What is it? Types Level Descriptors Abuse Side effects Risk Avoid Alternative meds Methods Misconceptions Too much Not enough Just right Controversies Hold Wake Did not give Gave too much

What is It?
What is pain exactly? This may seem like a simple question but it is important to define what it really is.
The International Association for the Study of Pain states that it is an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage.
It is estimated that more than 76 million people in the United States alone suffer from pain.
Different Types
The two different types of pain are called acute and chronic.
Acute pain is short lived. It does not last longer than six months. It is typically brought on from an injury. Once the injury has healed, it should go away completely.
Chronic pain is long lived. It is considered chronic once it lasts longer than six months. It may be brought on by tissue or nerve damage or various diseases such as cancer.
Pain Level
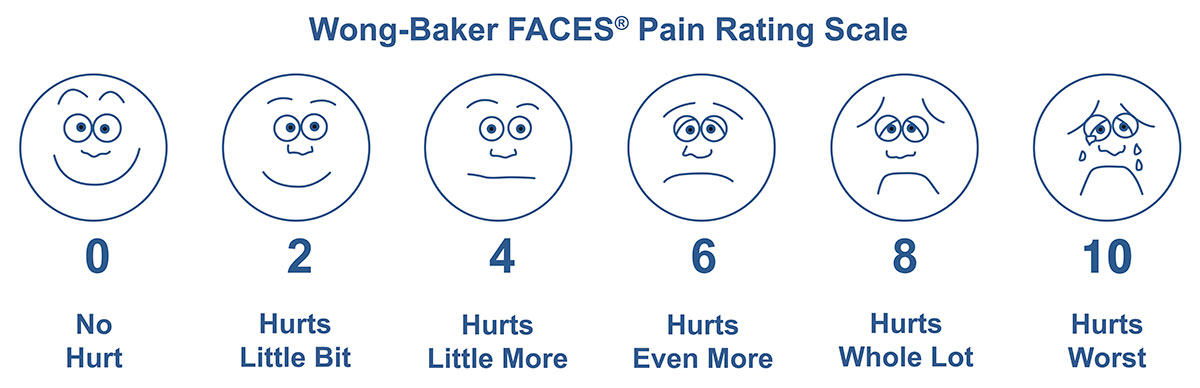
Pain level is usually based off of a 0-10 scale. 0 means the patient isn't experiencing any pain. 10 means they are having the worst pain they have ever experienced.
There is a well known graph with multiple faces called the Wong-Baker faces scale to ease the understanding of this concept (pictured above). People can often just point to the face to describe how they are feeling.
This scale is used before every pain medication I give while working as a nurse at the hospital. After the med is given, there is a reevaluation of the level to test the effectiveness of it. For ones given in oral (PO) form, this is done 45 minutes after. For the intravenous (IV) or intramuscular (IM) route, it is done 30 minutes after.
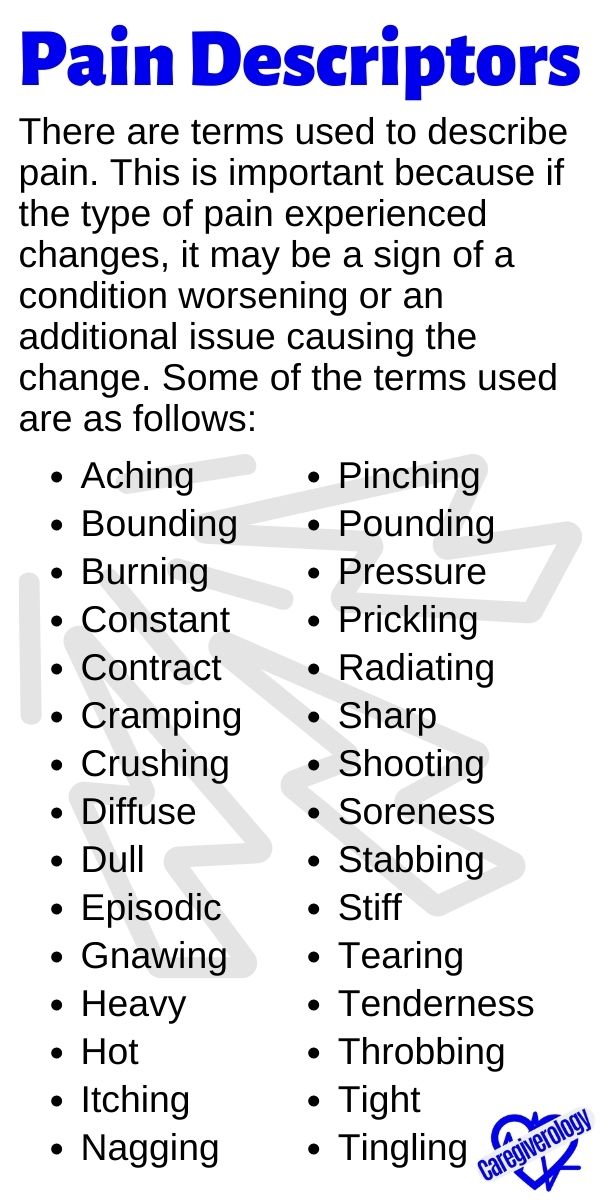
Pain Descriptors
There are also terms used to describe the pain. This is important because if the type of pain experienced changes, it may be a sign of the condition worsening or an additional issue causing the change. Some of the terms used are as follows:
|
|

Drug Abuse
Many people abuse drugs that are meant to control pain, such as prescription opioids or narcotics, to the point of ruining their lives and harming the lives of those around them. There are even consequences such as death from overdosing (OD) on various prescription pills.
There are even people who resort to crushing, mixing with water, and injecting the medications directly into their veins. That's not to mention all of the illegal drugs this type of addiction can lead to which often causes people to commit crimes just to support their habit.
This has led to an epidemic. There are millions of people addicted to various substances. Many of them started out as a visit to a hospital or a doctor's office. They never intended to create an addiction that would take over their lives and negatively affect the lives of those around them.
I have actually seen an increase in awareness of this problem. Pain medications are not given out as much or as easily as they used to be. People have started to fight back and try to reverse this problem we started. It won't be easy, and it probably won't fix all of the issues, but at least there is an attempt to make it right.
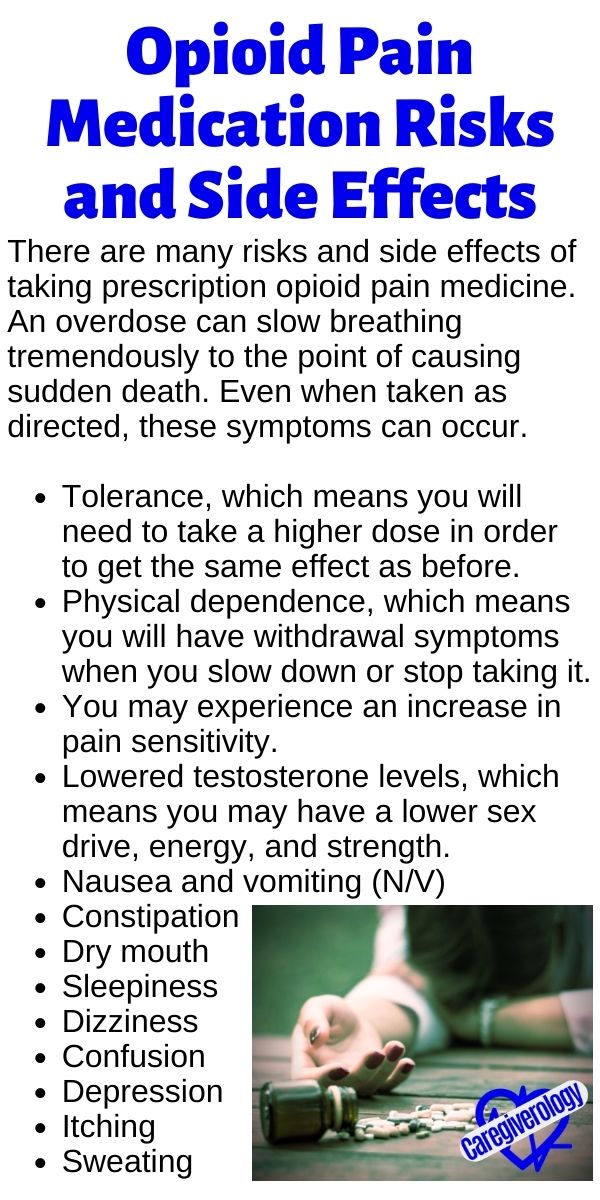
Risks and Side Effects
There are many risks and side effects of taking prescription opioid pain medicine. An overdose can slow breathing tremendously to the point of causing sudden death. Even when taken as directed, these symptoms can occur.
- Tolerance, which means you will need to take a higher dose in order to get the same effect as before.
- Physical dependence, which means you will have withdrawal symptoms when you slow down or stop taking it.
- You may experience an increase in pain sensitivity.
- Lowered testosterone levels, which means you may have a lower sex drive, energy, and strength.
- Nausea and vomiting (N/V)
- Constipation
- Dry mouth
- Sleepiness
- Dizziness
- Confusion
- Depression
- Itching
- Sweating
Even Greater Risk
People are at greater risk if they have the following:
- History of drug misuse, substance use disorder, or overdose
- Mental health conditions including depression and anxiety
- Sleep apnea
- Elderly age which includes people 65 years and older
- Pregnancy
What to Avoid
There are a few different things to avoid while taking prescription pain meds unless your health care provider approves such as:
- Alcohol of any kind
- Benzodiazepines (examples: xanax and valium)
- Muscle relaxants (examples: soma and flexeril)
- Hypnotics (examles: ambien and lunesta)
Alternative Medications to Opioids
Some alternatives to prescription medication includes:
- Over the counter (OTC) pain relievers (examples: acetaminophen (tylenol), ibuprofen (motrin), and naproxen (aleve)).
- Medications used for depression or seizures can sometimes provide relief.
- Physical therapy (PT) and exercise.
- Cognitive behavioral therapy where patients learn how to change physical, behavioral, and emotional triggers of pain and stress.
Alternative Methods
In addition to, or instead of medication, there are other ways to control pain. Depending on what is causing the pain, warm packs, heating pads, or cold/ice packs may be used. Just a simple ice pack (pictured below) can often work wonders. I've even seen people use things such as bags of frozen vegetables.
A machine sometimes used in hospitals is called a k pad (pictured below). They can be used for heat and cold depending on the way it is set up. I haven't seen them much lately but they used to be used often. Currently, there has to be a doctor's order to use one. There is a risk of applying too much heat so the orders often require breaks in between uses.
There are also relaxation and distraction techniques such as music and pet therapies. For many cases, emotional support and understanding can work wonders. Sometimes, just repositioning, whether it be by adjusting the head of the bed or the use of pillows can make a big difference.
A PCA pump (pictured below) is basically an IV that is connected to a pump that the patient can control themselves. Of course there are limitations to them, but instead of waiting hours in between getting medicated, they can get a smaller dose every few minutes if desired. I used to see these types of pumps being used fairly often, but not so much lately.
An epidural is a catheter that is placed directly into the spinal column. These are commonly used during childbirth however, I have seen them used in other cases as well. The medication is often given continuously at a very slow rate as to provide more consistent relief. These patients are usually monitored and charted on more carefully because there are risks to using this method.
 Ice pack
Ice pack PCA pump
PCA pump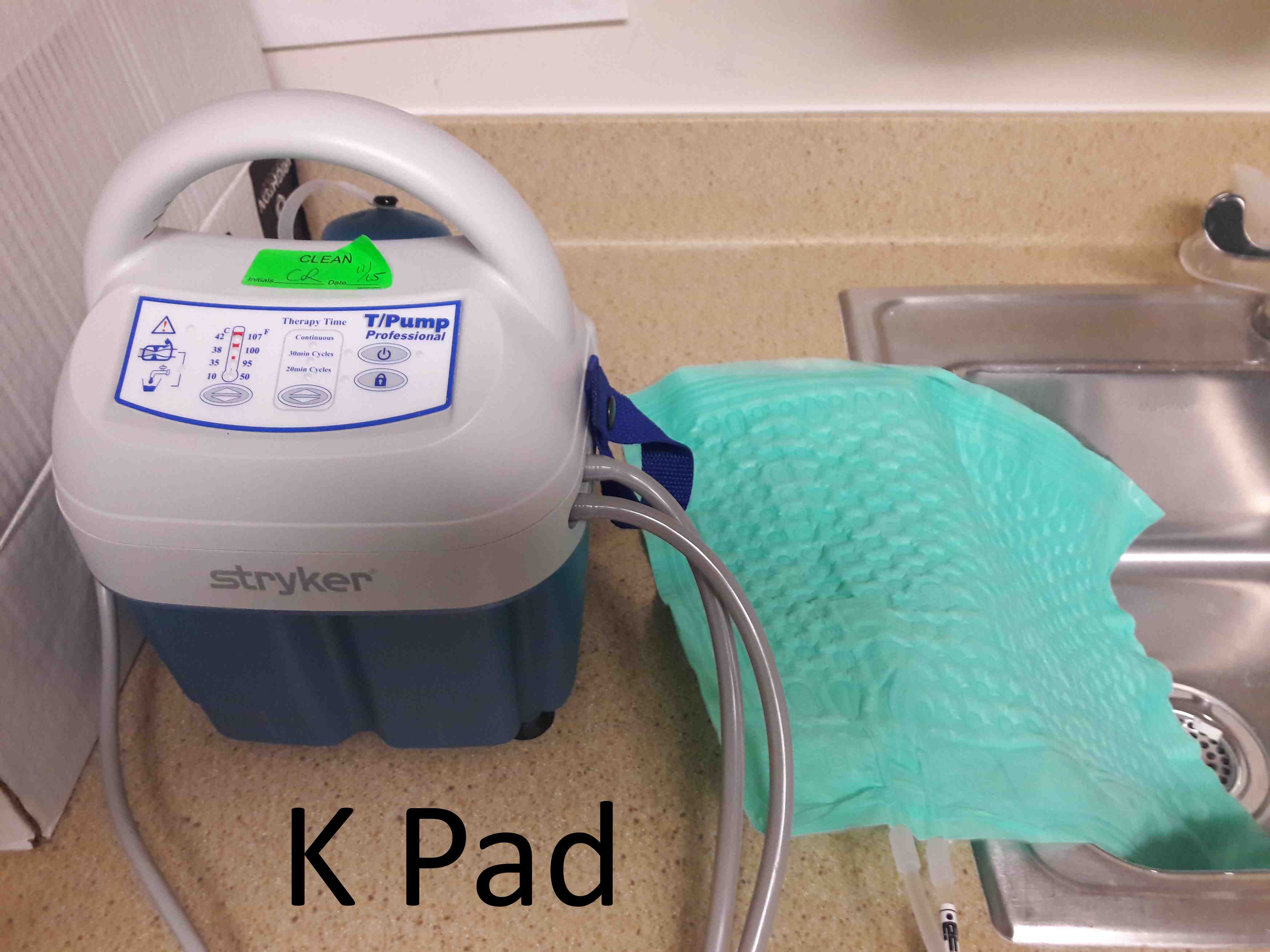 K pad
K pad3 Common Misconceptions
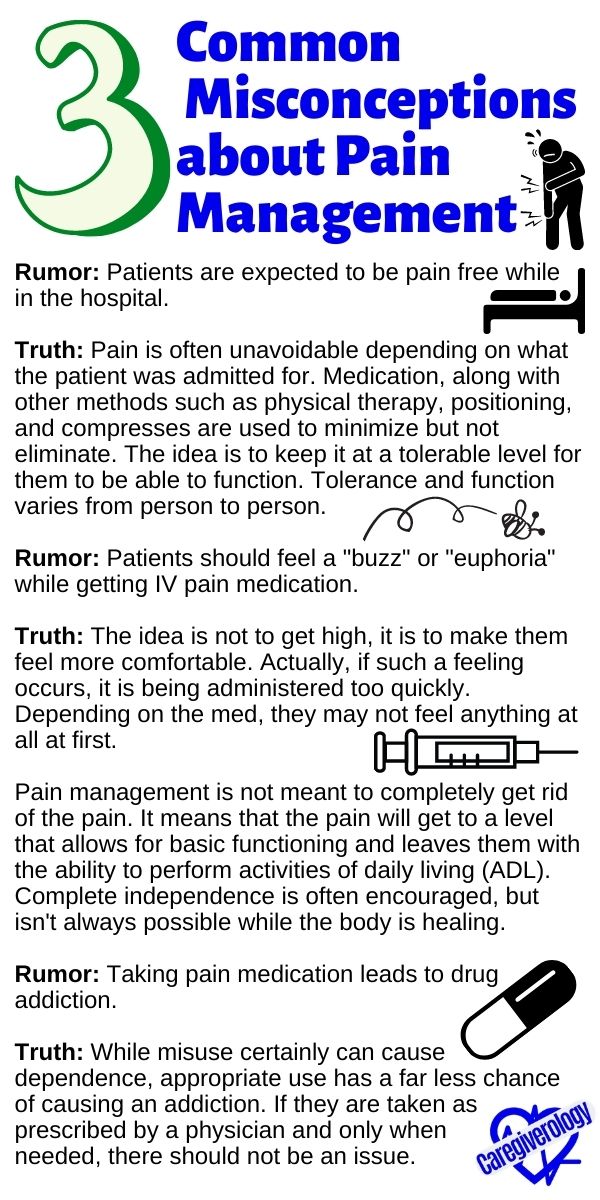
There are some common misconceptions when it comes to pain management. I will attempt to debunk a few of them here.
Rumor: Patients are expected to be pain free while in the hospital.
Truth: Pain is often unavoidable depending on what the patient was admitted for. Medication, along with other methods such as physical therapy, positioning, and compresses are used to minimize but not eliminate. The idea is to keep it at a tolerable level for them to be able to function. Tolerance and function varies from person to person.
Rumor: Patients should feel a "buzz" or "euphoria" while getting IV pain medication.
Truth: The idea is not to get high, it is to make them feel more comfortable. Actually, if such a feeling occurs, it is being administered too quickly. Depending on the med, they may not feel anything at all at first.
Pain management is not meant to completely get rid of the pain. It means that the pain will get to a level that allows for basic functioning and leaves them with the ability to perform activities of daily living (ADL). Complete independence is often encouraged, but isn't always possible while the body is healing.
Rumor: Taking pain medication leads to drug addiction.
Truth: While misuse certainly can cause dependence, appropriate use has a far less chance of causing an addiction. If they are taken as prescribed by a physician and only when needed, there should not be an issue.
Too Much
There is a risk of taking too much. If this does happen, it can result in:
- A critical decrease in heart rate, blood pressure, or respiratory rate
- An increase in drowsiness, over sedation, or physical dependence
- An increased risk of falling or re-injury
- Longer hospital stays and slower recovery time
Not Enough
With that being said, they shouldn't necessarily refuse to take pain medication. It is ultimately their decision but pain left untreated can lead to:
- A critical increase in heart rate, blood pressure, or respiratory rate
- An increase in sleeplessness and agitation
- Slowed healing
- Longer hospital stays and slower recovery time
Just Right
When taken as prescribed, it can
- Keep the pain at a tolerable level
- Lead to a faster recovery
- Shorten hospital stays and help avoid potential hospital acquired infections (HAI)
Common Controversies
There are controversial topics when it comes to pain management. Working in a hospital, I see these problems come up all of the time. The reactions vary from patient to patient and nurse to nurse.
Hold the Medication?
I've heard of pain medication being held because there was question if they were really needed it or not. Is this right? Should meds be held if there is suspicion that it is being abused? These can be very difficult questions for some.
Pain is subjective. It is often impossible to tell if someone is really hurting or not. Some people handle pain differently than others. Just because someone is smiling and laughing doesn't necessarily mean they aren't hurting.
People who suffer from chronic pain often have been coping with it constantly for years. It's something they just have to live with. Therefore, when they hurt, they don't always show it like someone who is suffering from acute pain.
This also causes them to have a higher tolerance to the medication which means they have to take more in order to get the same effect. This doesn't mean they are chasing a high they used to have or are trying to get rid of the pain completely.
It just means that over time, years for some, their bodies have gotten so used to what they've been taking, what might kill one person who never takes any pain medication, will barely affect the other person who has been struggling with it for most of their life.
Here is my personal opinion on the matter. If the medication has been prescribed by a physician and the vital signs are stable, there is no reason not to give it. It really doesn't matter if the nurse thinks one way or the other. I know there are others who would disagree with me, but I stand by that.

Wake them Up?
There is also the question of whether patients should be woken up at a specific time if requested when there is an as needed (PRN) pain med that can be given. This is a common one during night shift hours. If they are sleeping, they can't be in pain right?
Here's my take on it. Medication, especially ones that are taken orally (PO), can take quite some time in order to take effect. If it isn't given until the pain wakes them up, it can take quite awhile in order to get the pain back down to a therapeutic level. It needs to be addressed before it becomes overwhelming.
Some argue that if it's that important, the patient can set their own alarm. I can see both sides of that stance. But me personally, I usually just wake them up myself. I may change that in the future if I hear a compelling enough argument not to.
Example Where I Did Not Give
There have been instances, one I can think of in particular, where I did not give the PRN pain medication to a patient with stable vital signs. The reason? The patient was extremely lethargic, not just your average tired. They couldn't stay awake long enough to tell me what was hurting. They would also sit on the side of the bed from time to time, swaying back and forth, and nearly falling forward.
In this particular case, even though they were irate and demanding, I held the medication. I felt like I was doing the right thing, but there was that small part of me that wondered if I should've just given it. I spoke with other staff concerning the matter and they agreed that it should be held.
My judgment was confirmed to be right when I found out the next day that the patient had fallen off of the bedside commode (BSC). They were so lethargic that they fell asleep while trying to go to the bathroom. Even after this, they still demanded more pain meds and left against medical advice (AMA) when it wasn't given.
Example Where I Gave Too Much
There has been a case where narcan had to be given, which is the drug commonly given to reverse an overdose. I am forever grateful that the patient was on the heart monitor at the time. The telemetry monitor room called and told me the patient's oxygen level had dropped significantly.
Looking back and considering the circumstances, I should have never given it to begin with. In my defense, I had just started practicing as a nurse, but now I am quite a bit more careful. Controlling how much and how often, as well as close monitoring, really is important.
Medical References for Caregivers
From Pain Management for Your Patient to Home
References:
CDC Guideline for Prescribing Opioids for Chronic Pain - United States, 2016
Recent Articles
-
What to Expect During Post-Operative Recovery at Home - Caregiverology
Apr 08, 25 08:21 PM
Surgery may be over, but the journey to full recovery is just beginning, and for many people, the hardest part happens after they leave the hospital. -
How to Plan for Aging: Financial, Health, and Lifestyle Considerations
Mar 29, 25 12:40 PM
Did you know that 70% of people over 65 will need some form of long-term care? Yet, many delay planning until it’s too late. Aging is inevitable, but how we experience it depends on preparation. -
Speech Disorders: How to Know When It's Time to See a Professional
Mar 27, 25 07:05 AM
When it comes to human interaction, we need to be able to communicate effectively.




New! Comments
Have something to say about what you just read? Leave a comment in the box below.